Written by Luke Parkes
Introduction
Newborn screening (NBS) is an impactful public health initiative that enables the diagnosis of severe conditions in asymptomatic infants at birth. Typically, NBS programmes include testing for a select number of metabolic and genetic conditions via protein expression, with additional targeted screening for inherited conditions where there is a familial or community history of a disease. A new advancement in NBS currently being piloted in multiple countries (e.g. the United Kingdom and United States) is genomic screening via whole genome sequencing (WGS). Newborn genomic screening enables the diagnosis of hundreds of rare, treatable, genetically defined conditions that would otherwise require long diagnosis journeys leading to delayed intervention, and often resulting in irreversible clinical decline.
However, for the many genetic conditions that genomic NBS will allow early diagnosis for, the interaction with health technology assessment (HTA) agencies is potentially complex and consequential. The inclusion of a genomic condition in a NBS programme will likely affect a manufacturer’s planning, evidence generation, and economic modelling.
We have considered key implications for HTA from the perspective of submitting companies, and proposed steps that may be taken to prepare for the changes caused by the availability of genomic NBS.
Key implications for HTA
Increased heterogeneity in patient population
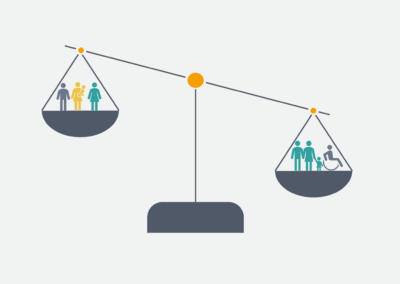
Genetic disorders often vary widely in severity and age of onset. Genomic NBS introduces further variability as both symptomatic and asymptomatic cases of a disease will be diagnosed. Individuals will therefore present with a wider range of baseline characteristics and disease severity. This heterogenous population may also meet differing treatment eligibility criteria, adding more complexity to the treatment pathway. An additional consideration is that not all parents or guardians may consent to genomic NBS, which may lead to a later diagnosis and potential equality issues around access to new treatments.
Companies should ensure that HTA evidence submissions address the full spectrum of patients who will be diagnosed, consider how that differs in the absence of NBS, and clearly highlight where new treatments may address equality issues arising from differing proportions of uptake in demographic groups.
Altered natural history
Genomic NBS can eliminate long diagnostic delays, enabling earlier management and treatment of diagnosed conditions, and individuals receiving earlier treatment may also have improved clinical outcomes. By avoiding the diagnostic odyssey and receiving earlier support and planning, quality of life (QoL), including the burden on mental health, may also be improved for both patients and caregivers.
Companies should explore the impact of presymptomatic diagnosis on baseline characteristics, health state distributions, treatment pathways, and subsequent prognosis. Market research and targeted literature reviews may help to clarify uncertainties in this regard.
Risk of overtreatment in asymptomatic patients
For some conditions (e.g. late onset Pompe disease [LOPD]), severity and age of onset cannot be predicted with available testing information. This means that treatment decisions will need to be made without clear prognostic indicators. In such situations, there is a risk of overtreatment, which may in turn increase the risk of treatment complications and reduced QoL without a clear corresponding benefit.
Companies may consider presenting starting and/or stopping rules to avoid overtreatment and to offset potentially increased costs due to longer treatment. These measures will improve cost-effectiveness and reconcile budget impact.
Improvement in efficacy of new treatments
Earlier treatment with new therapies may improve long-term outcomes and reduce overall healthcare costs. This is especially relevant where new treatments may prevent irreversible clinical decline and provide sustained/long-term stability. However, demonstrating these benefits in HTA submissions may be challenging due to limited data.
A clear strategy and supporting narrative should be developed in areas such as early disease treatment benefit and treatment-specific QoL improvements, supported by external evidence (see below).
Exacerbation of data paucity challenges
There may be limited clinical trial data for patients who are treated asymptomatically until NBS is well established and widely used. Therefore, estimating parameters such as disease progression rates or stability will be challenging. HTA bodies adopt flexibility in the evidence requirements for rare diseases; nonetheless, failure to capture data in people who are asymptomatic may lead to restrictions in HTA approvals or rejection of claims of early treatment benefit.
Structured expert elicitation and real-world evidence (in people who are asymptomatic) will be crucial in addressing data gaps and reducing uncertainty.
Conclusion
NBS-WGS will transform rare disease diagnosis and management in the countries that adopt it and will likely affect HTAs for new orphan technologies within the next decade.
Ultimately, infants with certain genetic or metabolic conditions who may not otherwise be diagnosed until symptoms appear stand to benefit greatly from the avoidance of long diagnostic delays and earlier intervention, particularly where treatments effectively halt or slow disease progression. Unfortunately, this presents many data challenges, as the shift in clinical care that genomic NBS may provide is not captured in the literature or pivotal clinical trials. Early planning will be crucial to characterise uncertainty around the impact of genomic NBS, as will engaging with HTA bodies to clarify data requirements and approaches to be taken. Where possible, evidence from patients treated or diagnosed asymptomatically should be presented, which may be available from early access schemes or registries.
If you would like to learn more about HTA submissions (including systematic reviews, health economic modelling, and medical writing), please contact us at Source Health Economics, a HEOR consultancy specialising in evidence generation, health economics, and communication.